More than a hundred years ago, disease immunizations often seemed like something out of a low-budget horror movie: Mix water with a sick patient’s pulverized scabs. Then, insert the pulp into shallow cuts on a healthy person’s arm.
Medicine has advanced since this mid-19th century process of variolation, used to inoculate against smallpox. Vaccines today are created in sterile labs and tested rigorously before being released to the general public.
But there is no vaccine available for the novel coronavirus, which has grown into a global pandemic. In the absence of widespread testing, the United States has turned instead to an older public health measure: isolation.
“For now, we have to rely heavily on social participation,” said University of Chicago historian Christopher Kindell, Ph.D.’19, a scholar of public health, mobility and race. “We’re watching people practice social distancing, which is similar in many ways to what was typical in the 19th century.”
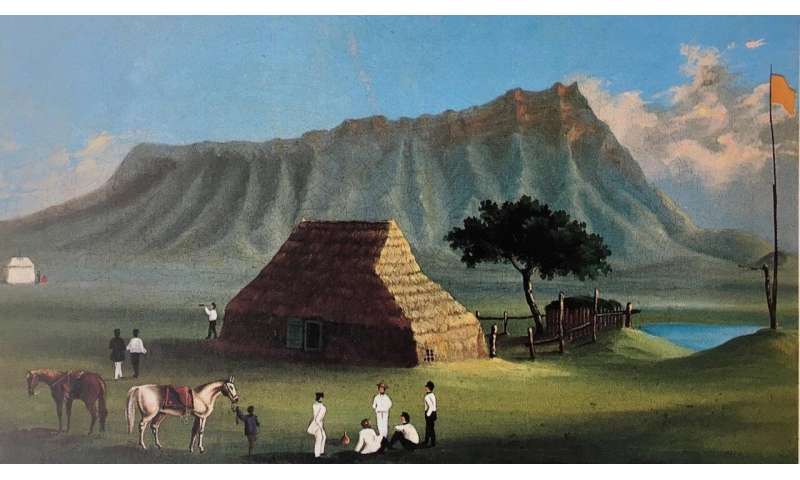
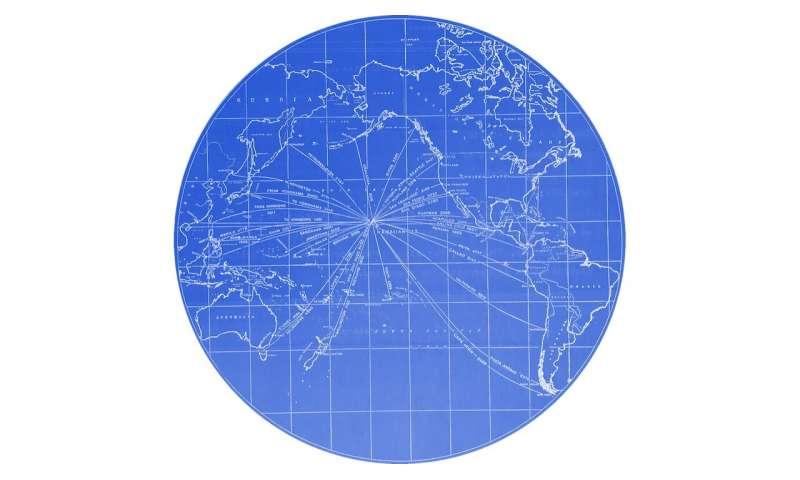
A UChicago postdoctoral fellow, Kindell’s current book project focuses on Hawaii’s role as a “sanitary sieve”—a disease-screening checkpoint as merchants, traders and laborers crossed the Pacific Ocean. Because 19th-century steamships rarely traveled long distances uninterrupted, Honolulu in particular became a vital international harbor for cargo from Hong Kong to San Francisco, or Sydney to Vancouver.
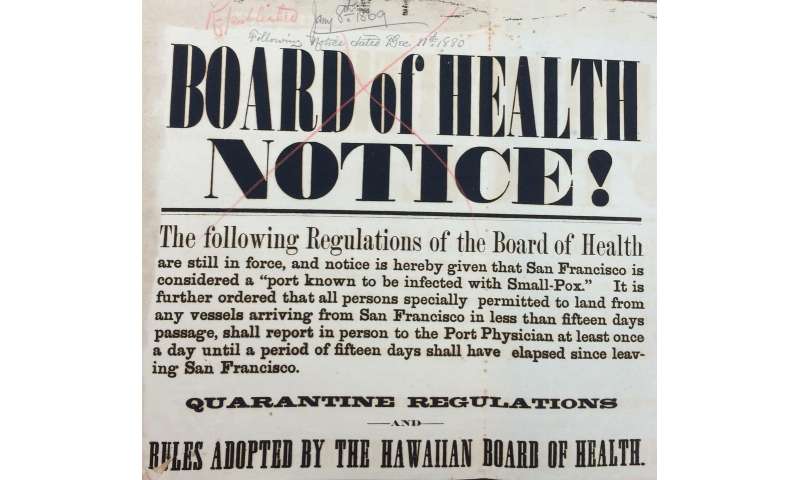
But that economic activity also overexposed Hawaii to diseases such as smallpox, cholera and the bubonic plague. Because immunization efforts produced mixed results—due to both medical limitations and cultural resistance to the practice—public health officials often turned instead to quarantines.
Even those weren’t always successful, Kindell said. Similar to today’s calls for social distancing, the effectiveness of quarantines depended on broad public cooperation.
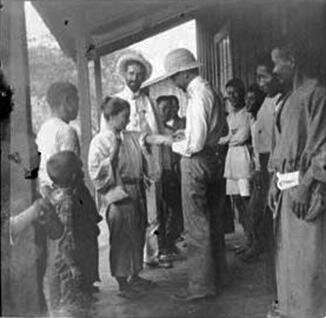
“People frequently avoided quarantine based on their socioeconomic status and race,” Kindell said. “For the wealthy, well-connected and white, it was often possible to escape maritime quarantine regulations. If you were the captain of a ship or a cabin passenger, disembarking from a vessel soon after its arrival wasn’t particularly difficult. If you were a migrant laborer or a steerage passenger, then your chances of getting out of quarantine were less promising.
“But typically, infectious diseases don’t recognize economic status. They don’t recognize gender. They don’t recognize race.”
Still, health officials at the time promoted the idea of diseases as “foreign,” stoking animus toward Chinese immigrants in particular. Those attitudes did little to protect island residents, as people from other countries continued to flow in.
“There were multiple waves of immigration from different places around the world, and everyone was susceptible,” Kindell said. “Classifying smallpox as a ‘foreign’ disease, or a ‘Chinese’ disease, really did everyone in Hawaii a disservice. You can’t protect an ethnically diverse public when you focus your attention on a single racial group.”
Honolulu saw its largest smallpox outbreak in 1853-54, when the disease killed at least 6,400 people—and, by some estimates, as many as 11,000. Smaller outbreaks in 1872 and 1880-81 posed less of a threat to Hawaiian lives, with 298 combined deaths reported, but the specter of disease still loomed for officials and the public at large.
“Civil servants in Honolulu were concerned about Hawaii’s international reputation,” Kindell said. “A single outbreak of smallpox—or cholera or bubonic plague—put the entire Pacific World at risk.
“But if Hawaiians could demonstrate that they had created a sound sanitary infrastructure—and that diseases were relatively rare in Honolulu as a result—then it made the archipelago more commercially important to everyone else.”
Fears of economic collapse are echoed today. In the face of ongoing COVID-19 outbreaks, state and local officials around the country have issued orders closing non-essential businesses. While those measures are necessary to help save lives, they have also wreaked havoc on restaurant workers, small business owners, and countless others who have seen their paychecks suddenly evaporate.
But officials have less control over the mobility of individuals—many of whom continue to ignore calls for social distancing.
For Kindell, such moments highlight the inherent fallibility of social isolation strategies.
Source: Read Full Article
