Researchers led by the University of Lausanne, Switzerland, have tested the impact of a digital clinical decision support algorithm (CDSA) called ePOCT+ on managing acutely ill children under 15 in Tanzanian primary care facilities. The goal was to compare the effects of using ePOCT+ versus usual care in reducing antibiotic prescriptions and assessing clinical outcomes.
In a paper titled “A digital health algorithm to guide antibiotic prescription in pediatric outpatient care: a cluster randomized controlled trial,” published in Nature Medicine, the team finds that ePOCT+ reduced antibiotic prescriptions without compromising clinical outcomes in acutely ill children.
Antibiotic resistance is a global health threat, responsible for millions of deaths annually.
Inappropriate antibiotic use contributes significantly to antimicrobial resistance (AMR), especially in regions like sub-Saharan Africa. The study aimed to see if ePOCT+ CDSA assistance could address the problem of antimicrobial resistance by safely reducing antibiotic prescribing to clinically recommended guidelines.
A cluster randomized controlled trial was conducted in Tanzanian primary care facilities. Over 44,000 consultations were included, with facilities randomly assigned to ePOCT+ or usual care.
Use of the ePOCT+ CDSA significantly reduced antibiotic prescriptions compared to usual care (23.2% vs. 70.1%). Safety outcomes such as death and non-referred secondary hospitalizations by day 7 showed no significant difference. Reducing antibiotic over-prescription aligns with Tanzania’s efforts to curb antibiotic use for long-term safety.
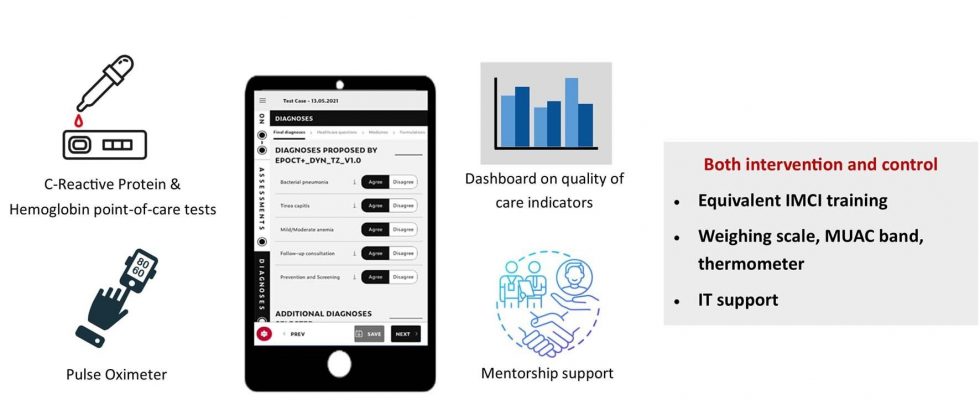
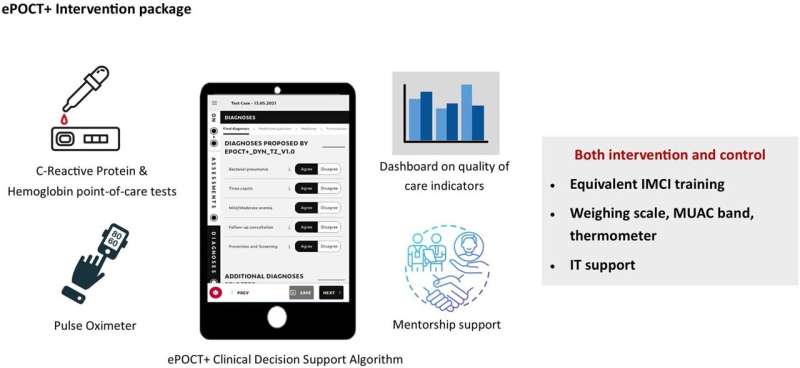
CDSAs, like ePOCT+, have been designed to serve as expert troubleshooters and decision trees to assist medical staff by generating prompts and reminders based on patient data. The digitized tool combines an individual’s health information with the health worker’s observations and clinical protocols to assist in making both diagnosis and treatment decisions.
As CDSAs become more efficient in analyzing patient data, they can reduce barriers to quality of care from a lack of access to specialists and help even experienced health care workers better follow evidence-based clinical recommendations for diagnosing and treating patients.
A typical mechanical troubleshooter follows a logic tree with “yes” or “no” questions and diagnostic tests. This is a way of quickly narrowing down the components of a system that are failing. In a car repair scenario, it would not matter that the vehicle also has a flat tire when looking into an electrical problem, but things like year, make, and model would be crucial.
Knowing a human patient’s year, make, and model is also crucial. While the current study found success, the CDSA was tailored to advise specifically on children and was not optimized for pregnant women or elderly patients with suppressed immunity.
As the biological systems of the human machine tend to be much more interrelated than mechanical systems, health history and current comorbidities are needed to understand how best to offer treatment. Each of these data points then requires intensive analysis and consensus from medical experts to provide the underpinning of the CDSA decision tree.
For CDSAs to operate successfully, they need to be integrated with reliable patient information and have optimized thresholds for when they have enough data to proceed. They also require local clinical knowledge, such as the prevalence of a disease in the corresponding patient population, to avoid over-testing for unlikely diseases with shared symptom profiles.
Ultimately, the obstacles to achieving trustworthy and reliable CDSAs may seem daunting. The alternative is relying on whatever level of expertise the local human health care worker happens to have in diagnosing and treating illness without such a tool. This makes the effort being put into CDSAs seem urgent and long overdue.
More information:
Rainer Tan et al, A digital health algorithm to guide antibiotic prescription in pediatric outpatient care: a cluster randomized controlled trial, Nature Medicine (2023). DOI: 10.1038/s41591-023-02633-9
Journal information:
Nature Medicine
© 2023 Science X Network
Source: Read Full Article