TOPLINE:
Among patients with diabetes and without known coronary artery disease and referred for myocardial perfusion imaging, 12.7% had significant ischemia, and 60% had reduced myocardial blood flow reserve (MBFR) including those without symptoms of ischemia. One third of these asymptomatic individuals had coronary microvascular dysfunction, and reduced MBFR was highly prognostic for mortality.
METHODOLOGY:
-
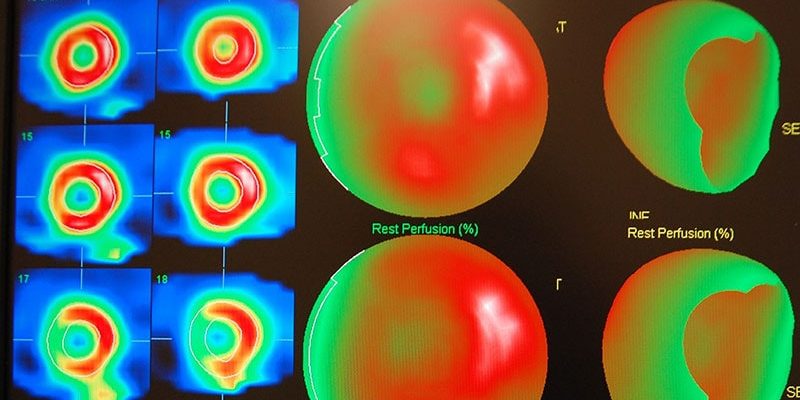
This retrospective, observational study included 2730 consecutive patients with diabetes and without known coronary artery disease treated in a large health system in the bi-state Kansas City metro area during 2010-2016 who underwent pharmacologic rest/stress myocardial perfusion imaging (MPI) using rubidium-82 positron emission tomography.
-
The cohort included 2083 (76%) people who had symptoms of suspected ischemia and 647 (24%) who were asymptomatic.
-
Researchers calculated MBFR as the ratio of myocardial blood flow at stress to flow at rest for the entire left ventricle.
-
Researchers developed univariate and multivariable Cox proportional hazards models to assess the association of abnormal MPI variables with all-cause mortality in the overall population and in symptomatic and asymptomatic patients with diabetes. The multivariate models adjusted for demographic characteristics, clinical risk factors, and other variables.
TAKEAWAY:
-
The study participants without symptoms had significantly higher prevalence rates compared with those with symptoms of perfusion defects (29.7% vs 22.6%), ischemia (30.5% vs 22%), and significant ischemia (12.5% vs 9%).
-
The overall study cohort had 461 (17%) deaths over a median of 2.93 years of follow-up, with a 17% rate among those with symptoms and 18% rate in those with no symptoms.
-
Older age, inpatient status, insulin use, reduced left ventricular ejection fraction at rest, and reduced MBFR were each independently associated with increased all-cause mortality among both symptomatic and asymptomatic people with diabetes.
-
The extent of ischemia did not significantly associate with all-cause mortality after accounting for MBFR in those with or without symptoms.
-
Every 0.1 unit decrease in global MBFR was associated with a significant 8% increased hazard of death among people without symptoms and a significant 9% increased hazard of death among those with symptoms.
IN PRACTICE:
“Future work is needed to study whether treatment of reduced MBFR identified on screening asymptomatic high-risk patients with diabetes improves outcomes,” conclude the investigators.
SOURCE:
The study was run by researchers at several US centers; the first author was from the Icahn School of Medicine at Mount Sinai in New York City. The report appeared online on October 18 in JACC: Cardiovascular Imaging.
LIMITATIONS:
Limitations for this study included potential referral bias — especially among asymptomatic people who generally are not referred for imaging when high-risk features are missing — and no information on duration of diabetes, quality of glycemic or lipid control, renal function, or diabetic end-organ damage, which are all factors that could help stratify risk in asymptomatic people with diabetes.
The analysis considered insulin use a surrogate marker for a more severe phenotype of diabetes.
Despite adjustment for many potential confounders as covariates, the observational nature of the study makes it subject to residual confounding.
Researchers did not have information on subjective outcomes such as nonfatal myocardial infarction. And researchers were not able to evaluate the effect of ischemia- or MBFR-guided revascularization in people with asymptomatic diabetes due to the low number of revascularization events in this group.
DISCLOSURES:
The study received no commercial funding. Several of the authors had individual disclosures detailed in the published report.
Mitchel L. Zoler is a reporter with Medscape and MDedge based in the Philadelphia region. Follow him at @mitchelzoler.
For more diabetes and endocrinology news, follow us on X (formerly known as Twitter) and on Facebook. You can also follow Medscape on Instagram, YouTube, and LinkedIn.
Source: Read Full Article