A recent study on healthcare workers in Japan has evaluated vaccine-induced humoral and cellular immunity against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) six months post BNT162b2 (Pfizer-BioNTech, USA) vaccination.
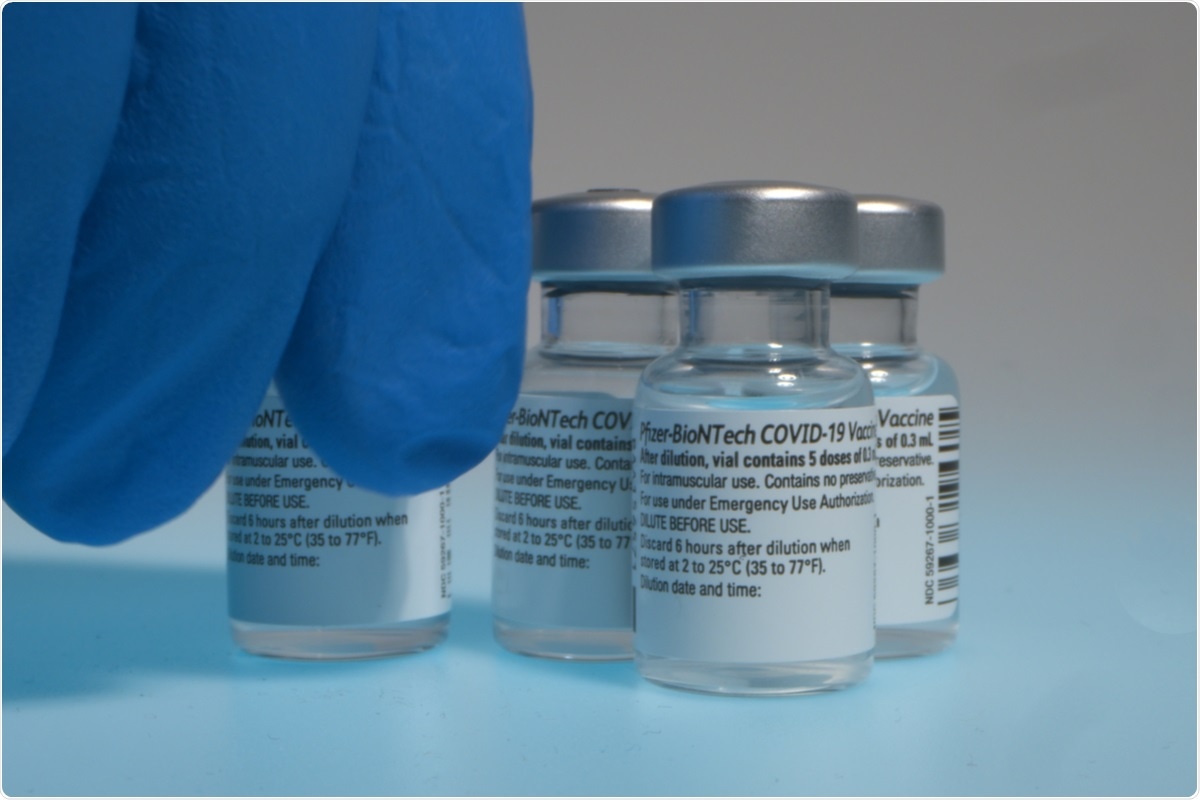 Study: Vaccine-induced humoral and cellular immunity against SARS-CoV-2 at 6 months post BNT162b2 vaccination. Image Credit: cortex-film/ Shutterstock
Study: Vaccine-induced humoral and cellular immunity against SARS-CoV-2 at 6 months post BNT162b2 vaccination. Image Credit: cortex-film/ Shutterstock
The research team observed a sharp decline in IgG antibodies specific to spike protein (SP) six months post-vaccination compared to the levels at three weeks after the second vaccine dose. However, the decline in the humoral index is weakly correlated to the observed cellular immune response.
A pre-print version of the research paper is available on the medRxiv* server while the article undergoes peer review.
Background
Vaccination has provided a powerful strategy to control the coronavirus disease-2019 (COVID-19) pandemic. Pfizer-BioNTech’s BNT162b2 vaccine became the first to receive emergency validation from the World Health Organization (WHO) for use against SARS-CoV-2.
Phase 3 trials of most vaccines exhibited high efficacies. However, the reports pointing at the long-term decline in vaccine efficacy and the occurrence of breakthrough infections have created a major concern across the globe. Reportedly, most vaccines exhibit declining efficacies six months after the vaccination. However, the potency of a vaccine in preventing severe disease is reported to persist at high levels.
The decline in vaccine effectiveness can be attributed to the decrease in antibody titers or humoral immunity. However, cellular immunity might as well be holding an even bigger role in prevention from severe COVID-19 than yet understood.
What did the researchers do?
The study was conducted on 98 healthy healthcare workers from Yokohama City University Hospital, Japan, who had undertaken two doses of the BNT162b2 vaccine from March to April 2021.
The team determined the SP immunoglobulin (IgG) levels against SARS-CoV-2 by using chemiluminescent enzyme immunoassay (CLEIA) at six months after vaccination. Data on SP IgG index titers of early weeks from this study were also compared with the observations at six months.
Later, a 50% neutralizing titer (NT50) was calculated from the neutralizing titer assay that utilized an HIV-based pseudovirus bearing the SARS-CoV-2 spike.
In addition, SARS-CoV-2-specific T-cell response in the form of spot forming cell counts (SFC) was evaluated by interferon (IFN)-γ ELISpot assay to assess the status of cellular immunity at six months after vaccination.
What did the researchers find?
Humoral immune index
The team observed a surprising decrease in antibody titers, with only 1/15 titers noted at six months compared to those at three weeks post-BNT162b2 vaccine’s second dose. The geometric mean titers (GMT) of SP-specific IgG declined from 95.2 (95% confidence interval (CI); 79.8–113.4) at three weeks after vaccination to just to 5.7 (95% CI; 4.9–6.7) at six months.
A similar trend was noted for NT50, which also depicted a marked decrease in GMT from 680.4 (95% CI; 588.0–787.2) at three weeks to 130.4 (95% CI; 104.2–163.1) at 6 months.
There were four patients with a history of breakthrough infections that occurred after completing the second vaccine dose. In these, the SP IgG index titers ranged from 146.1 to 459.1, while NT50 ranged from 1631 to 8756 at six months. High antibody titers observed in these patients are believed to be induced by the breakthrough infection instances.
The team observed a negative correlation between the SP IgG index titer and alcohol consumption. The GMT of SP IgG index titer among non-drinkers was significantly higher than that among current drinkers {7.57 (95% CI 5.89, 9.73) vs. 5.34 (95% CI 3.37, 8.44)}. In addition, multivariable regression analysis revealed that age was another factor negatively correlated with the SP IgG index titer.
Cellular immune index
The correlation between cellular immunity, assessed by the SP-specific T-cell response, and humoral immunity, measured by SP IgG index titer, was weak, pointing to a different dynamic for a cellular immune response from the humoral.
A previous study had reported 184 SFC/106 peripheral blood mononuclear cells (PBMCs), a measure of SP-specific T-cell response, immediately after BNT162b2 vaccination. The SP-specific T-cell response observed in the present study was 84 SFC/106 PBMCs at six months after vaccination. The decline in cellular immunity was slower than that of antibody titer, indicating it to be less negatively correlated with age, possibly explaining its long-term effect in protecting from developing the severe form of this disease.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Ryo A, et al. (2021) Vaccine-induced humoral and cellular immunity against SARS-CoV-2 at 6 months post BNT162b2 vaccination. medRxiv. doi: https://doi.org/10.1101/2021.10.30.21265693, https://www.medrxiv.org/content/10.1101/2021.10.30.21265693v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Alcohol, Antibodies, Antibody, Assay, Blood, Cell, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Enzyme, Healthcare, HIV, Hospital, Immune Response, immunity, Immunoassay, Immunoglobulin, Interferon, Pandemic, Protein, Pseudovirus, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, T-Cell, Vaccine

Written by
Namita Mitra
After earning a bachelor’s degree in Veterinary Sciences and Animal Health (BVSc) in 2013, Namita went on to pursue a Master of Veterinary Microbiology from GADVASU, India. Her Master’s research on the molecular and histopathological diagnosis of avian oncogenic viruses in poultry brought her two national awards. In 2013, she was conferred a doctoral degree in Animal Biotechnology that concluded with her research findings on expression profiling of apoptosis-associated genes in canine mammary tumors. Right after her graduation, Namita worked as Assistant Professor of Animal Biotechnology and taught the courses of Animal Cell Culture, Animal Genetic Engineering, and Molecular Immunology.
Source: Read Full Article
