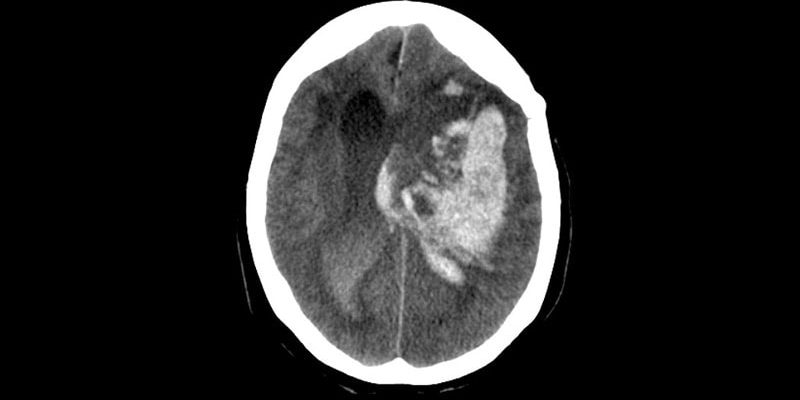
A combination of simple interventions for acute patients with stroke due to intracerebral hemorrhage (ICH) has been shown to significantly improve the chances of survival without major disability.
The INTERACT3 study showed that timely administration of a care bundle that included early intensive lowering of systolic blood pressure, strict glucose control, treatment of fever, and rapid reversal of abnormal anticoagulation led to less disability, lower rates of death, and better overall quality of life.
“This is a groundbreaking result. It is the first-ever published trial in ICH patients to show a clear benefit on functional outcomes and on mortality,” lead investigator Craig Anderson, MD, director of global brain health at the George Institute, Sydney, Australia, told theheart.org | Medscape Cardiology.
“These results show that if we can organize care and focus on optimal management of these four aspects of the health of the patient, they do better,” Anderson said.
“Game Changer”
“This is a game changer because now we have level A evidence showing something is definitely beneficial for these patients.” Anderson added. “That means hospitals have the imperative to organize their systems to do these things and maximize care. We have never had that before.”
Anderson noted that while some previous studies have suggested benefit from various interventions, such as early lowering of blood pressure, the results have not been conclusive.
“This means the intervention has not always been implemented, leading to large variations in clinical practice. But now we have a package that is proven to work, this should become a guideline-recommended practice,” he commented.
The INTERACT-3 results were presented on May 25 at the European Stroke Organisation Conference in Munich, Germany. They were also simultaneously published online in The Lancet.
Anderson explained that, until now, there haven’t been any proven treatments for ICH. “There has been a lot of energy and research put into the field, but this has resulted in several interventions that are ‘probably useful’ or which have a level B recommendation,” he said. “No therapy has been shown to be beneficial in a totally conclusive way, so we are still not entirely sure exactly whether the treatments we use actually make a difference.”
The INTERACT3 researchers therefore decided to evaluate a care package consisting of a bundle of several treatments in the hope that they may have additive or synergistic effects.
The study involved 7036 patients with imaging-confirmed spontaneous ICH who presented within 6 hours of symptom onset to one of 121 hospitals in 10 mainly low- and middle-income countries: Brazil, China, India, Mexico, Nigeria, Pakistan, Peru, Sri Lanka, Vietnam, and Chile.
Using a cluster design, all hospitals started with usual care as a control and then at some point during the study started using the care bundle intervention.
The care bundle protocol included the early intensive lowering of systolic blood pressure (target, <140 mm Hg), strict glucose control (target, 6.1 – 7.8 mmol/L in those without diabetes and 7.8 – 10.0 mmol/L in those with diabetes), antipyrexia treatment (target body temperature, ≤37.5° C), and rapid reversal of warfarin-related anticoagulation (target international normalized ratio, 1.5) in patients for whom these variables were abnormal.
Overall, the modified intention-to-treat population included 3221 patients who were assigned to the care bundle group and 3815 who were assigned to the usual care group. Primary outcome data were available for 2892 patients in the care bundle group and 3363 patients in the usual care group.
The primary outcome was functional recovery, measured with the Modified Rankin Scale at 6 months. Results show that the likelihood of a poor functional outcome was lower in the care bundle group (common odds ratio, 0.86; P = .015).
Patients who received the interventional care bundle also had a significantly lower rate of serious adverse events (16.0% vs 20.1%) and mortality (14.1% vs 17.0%).
NNT of 35 to Save One Life Free of Disability
“The number needed to treat (NNT) is just 35 to save a life free of disability,” Anderson commented. “That’s pretty good. We estimate that this care bundle would save tens of thousands of lives a year if universally adopted.”
The intervention group also spent less time in hospital and had improved health-related quality of life.
Anderson pointed out that the interventions included in the care bundle were all relatively easy to perform.
“They just require a bit more nursing time and the use of a few inexpensive medicines and maybe infusion pumps, but we’re not talking about the need for skilled surgery or a new therapy costing hundreds of thousands of dollars, so this care bundle should be very straightforward to implement. While we haven’t done a formal cost-effectiveness analysis, I would say it will definitely be good value for money.”
Anderson believes the rapid lowering of blood pressure is a very important part of the care bundle. He noted that target levels were achieved, on average, in 2.3 hours, compared to 4.0 hours in the control group. But he stressed that this was not just a trial of blood pressure reduction and that the whole package is important.
He gave a couple of possible reasons why this trial was successful whereas previous trials did not show a clear benefit of blood pressure lowering in ICH.
“Firstly, it was a very large trial with more than 7000 patients ― that is more than three times larger than any other trial in ICH. And secondly, the package of care means there are several different interventions that together show a real benefit,” he said. “It’s like the polypill, or a rehabilitation program ― if you put several different things together, the whole package can show really positive results.”
Anderson also pointed out that the study included a wide spectrum of ICH patients, and the benefit of the care bundle was seen across all groups and all stroke severities.
“There were a lot of patients with a large ICH, and if anything, they showed an even larger benefit with the bundle of care,” he said.
The researchers note that the burden of ICH is greatest in low- and middle-income countries. In 2019, 30% of all stroke cases in these countries were ICH, almost double the proportion seen in high-income countries (16%). This is in part due to high rates of hypertension and limited resources for primary prevention, including identification and management of stroke risk factors by healthcare services.
“Outstanding Example” of Less Therapeutic Negativity
Lili Song, MD, PhD, joint lead author and head of the Stroke Program at the George Institute China, said, “A lack of proven treatments for ICH has led to a pessimistic view that not much can be done for these patients.
“However, with INTERACT3, we demonstrate on a large scale how readily available treatments can be used to improve outcomes in resource-limited settings,” she said. “We hope this evidence will inform clinical practice guidelines across the globe and help save many lives.”
In a comment that accompanied the article, Wendy Ziai, MD, Matthew Bower, MD, and Daniel Hanley, MD, Johns Hopkins University, Baltimore, say the INTERACT3 study shows that “an intracerebral hemorrhage care bundle focused on physiological control interventions, whether synergistic or not, might promote better outcomes in hospitals where care has not previously optimized sustained interventions.”
Pointing out that the care bundle has minimal risks of cost and coordination and a high public health effect, they conclude: “This effort is an outstanding example of why less therapeutic negativity, and more intervention might benefit survivors of intracerebral hemorrhage.”
The INTERACT3 study was funded by the Department of Health and Social Care, the Foreign, Commonwealth and Development Office, the Medical Research Council, and the Wellcome Trust (all in the UK), the West China Hospital Outstanding Discipline Development 1–3-5 Programme, the National Health and Medical Research Council of Australia, Sichuan Credit Pharmaceutical, and Takeda (China).
European Stroke Organisation Conference (ESOC) 2023: Presented May 25, 2023.
Lancet. Published online May 25, 2023. Full text, Comment
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube
Source: Read Full Article