Probiotic-based therapeutic approaches are relatively new to the field of clinical dentistry. According to a recent review published in Frontiers in Dental Medicine, probiotic-based therapy in conjunction with established treatment regimens can effectively combat gingivitis and periodontitis.
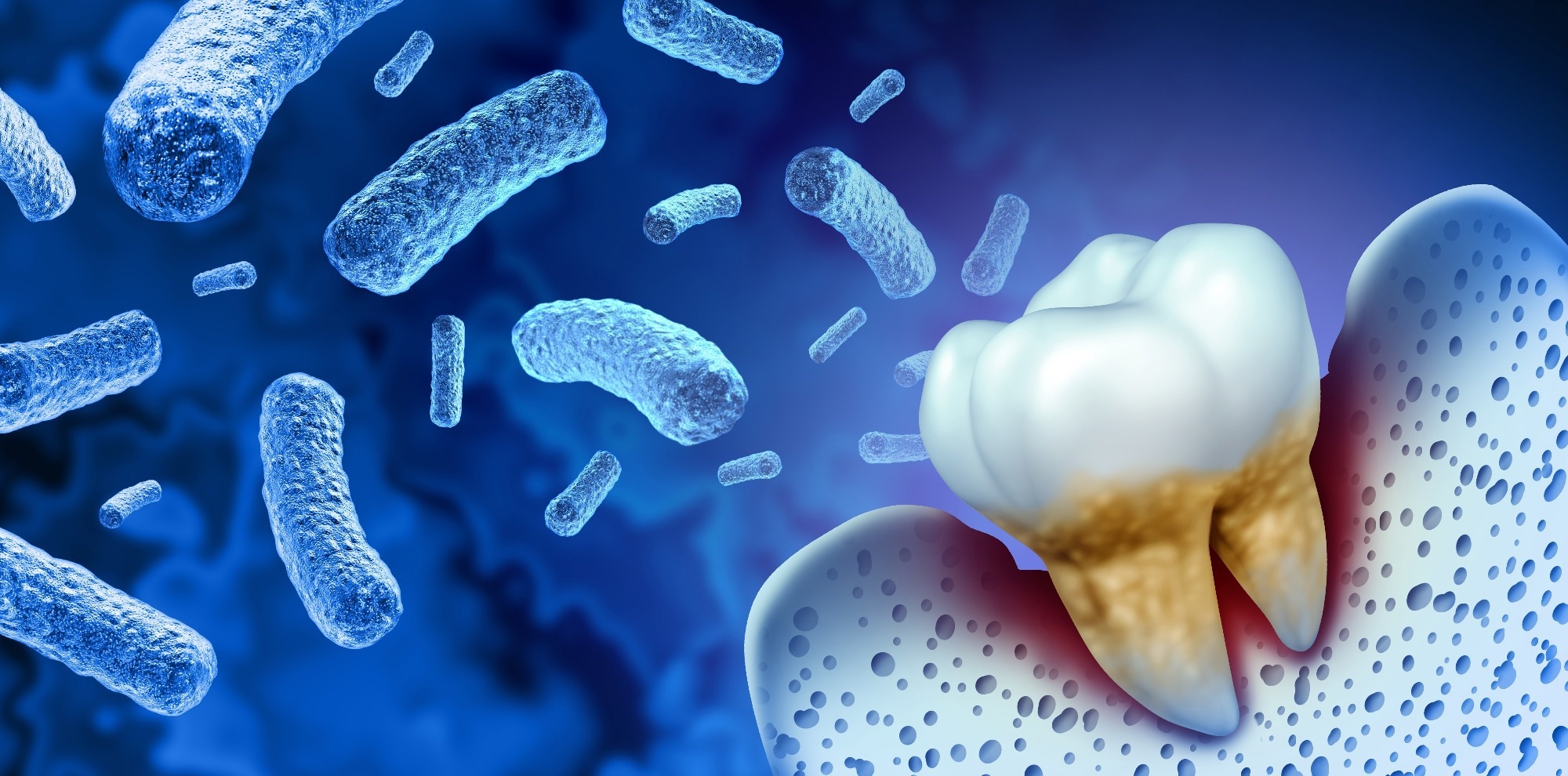 Study: Probiotics in the Management of Gingivitis and Periodontitis. A Review. Image Credit: Lightspring/Shutterstock
Study: Probiotics in the Management of Gingivitis and Periodontitis. A Review. Image Credit: Lightspring/ShutterstockOral microbiome
The human microbiome consists of millions of microorganisms that inhabit various body parts, including the gut, oral cavity, skin, and mucosa. The oral microbiome is the second largest microbial community in humans after the gut microbiome. The oral epithelia are infested with many bacteria, forming the bacterial biofilm.
For decades, scientific efforts have been directed toward investigating bacterial pathogens. A healthy host’s microbiota comprises commensals as well as certain pathogens. Concerning clinical dentistry, oral microbiota is deemed a health risk. Indiscriminate removal of oral bacterial biofilms has been an essential component of even the most recent therapeutic recommendations for preventing caries and treating periodontitis.
Probiotics: Mechanism, safety, and commercial aspect
Probiotics are beneficial microbes that modulate the immune response, provide a source of essential nutrients, and inhibit the proliferation and virulence of infectious agents. Probiotics interfere with the growth and metabolism of competing microorganisms via two mechanisms. The first method involves specific interference, in which bacteriocines (peptides) eradicate competing bacteria or alter their metabolism, thus impeding biofilm formation. A second mechanism is indirect interference, in which microbial competitors are destroyed by inducing nitrosative, oxidative, or acidic stress.
Further, probiotics influence their hosts locally and systemically by enhancing epithelial integrity, stimulating dendritic cell recruitment of regulatory T cells, and activating systemic oxytocin production. It was reported that probiotic lactobacilli could adhere to the gut mucosal lining and oral epithelia, which brings them near to human cells.
Evidence suggests that indiscriminate, medically unsupervised probiotic use is associated with various metabolic interferences with the human microbiota. It is considered safe to consume probiotics for systemically healthy individuals; however, it may be prudent to use only products with a validated safety profile for the specific purpose.
Probiotics are not recognized medications in the European Union (EU) or the United States. Instead, they are considered food supplements. In 2011, the European Food Safety Authority (EFSA) prohibited endorsing health claims for any commercial probiotic product sold in Europe due to a widespread lack of scientific evidence matching their efficacy standards.
Consumption of two bacterial supplements containing different strains of the same species of bacteria may significantly impact the microbiota and the host. Due to the interactions’ complexity, excessive amounts of probiotic dietary supplements with potentially conflicting properties are not recommended.
Probiotics in the management of oral health problems
Antibodies eBook
A growing number of randomized controlled trials (RCTs) are underway to evaluate the benefits of probiotics in treating oral health issues such as gingivitis and periodontitis. In the present review, 36 RCTs (published between 2009 and 2021) were reviewed to understand the utility of probiotics-based therapy for managing oral health problems.
The most often studied probiotic was a combination of two probiotic Lactobacillus reuteri strains, employed in 17 of the 36 RCTs assessed, followed by various other common probiotics.
The probiotics dosages delivered (in the form of a lozenge, yogurt, or toothpaste) as a single application ranged from 108 to 109 colony forming units (CFU), with a bandwidth ranging from 3 x 103 CFU to 6.5 x 109 CFU – which were administered for 3-12 weeks.
Probiotics in the management of chronic gingivitis and periodontitis
Several studies delineated that probiotics dramatically reduced gingival inflammation as an adjuvant to effective mechanical plaque management; however, only moderate effects were reported in others. In study cohorts with insufficient mechanical plaque control or experimental gingivitis trials, the outcomes remained equivocal. On the other hand, in RCTs with the same L. reuteri probiotic use, subjects with poor dental hygiene with clinical symptoms of chronic gingivitis were investigated. The probiotic use led to significant reductions in gingival inflammation despite little or no improvements in oral hygiene measures.
The results of the periodontitis trials are not as consistent and uniform; in some studies, no additional benefits were identified. Most RCTs that used the L. reuteri probiotics and incorporated mechanical oral prophylaxis measures reported substantial improvements––relating to pocket closure and periodontal inflammation reduction compared to placebo. Additionally, Bifidobacterium lactis HN019 use conferred markedly better pocket closure and periodontal inflammation reduction benefits. While 12-week probiotic lozenge intake containing heat-killed Lactobacillus plantarum L-137, improved the Th1 helper cell-induced immune response and also aided in gaining reduced residual pocket depth in periodontal recall patients.
The findings of currently available meta-analyses and systematic reviews on the probiotics-based treatment of gingivitis or periodontitis are mixed. The available indicates – "no additional benefit for pocket reduction"; "limited benefits in attachment gain or pocket closure of deeper pockets"; or "minimal gingival inflammation reduction."
The findings suggested that probiotic administration may be an important component of innovative, targeted treatments for periodontitis and gingivitis. An RCT indicated that probiotic use can help in controlling inflammation on both, local and systemic levels and may aid in preventing the development of bacterial dysbiosis.
Conclusion
Certain questions regarding the use of probiotics in the treatment of gingivitis and periodontitis remain unanswered. Meanwhile, guidelines based on broad consensus specifying the selection of the appropriate probiotic, dosage, and duration of administration are lacking. RCTs investigating the benefits of probiotic use in clinical dentistry can add a valuable element to the available therapeutic options.
- Schlagenhauf, U., & Jockel-Schneider, Y. (2021). Probiotics in the management of gingivitis and periodontitis. A review. Frontiers in Dental Medicine. doi: 10.3389/fdmed.2021.708666 https://www.frontiersin.org/articles/10.3389/fdmed.2021.708666/full
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Bacteria, Biofilms, Cell, Chronic, Dendritic Cell, Dental Hygiene, Dentistry, Dysbiosis, Efficacy, Food, Food Safety, Gingivitis, heat, Hygiene, Immune Response, Inflammation, Lactobacillus, Medicine, Metabolism, Microbiome, Nutrients, Oral hygiene, Oxytocin, Peptides, Periodontitis, Placebo, Probiotic, Probiotics, Proliferation, Prophylaxis, Skin, Stress, Supplements

Written by
Nidhi Saha
I am a medical content writer and editor. My interests lie in public health awareness and medical communication. I have worked as a clinical dentist and as a consultant research writer in an Indian medical publishing house. It is my constant endeavor is to update knowledge on newer treatment modalities relating to various medical fields. I have also aided in proofreading and publication of manuscripts in accredited medical journals. I like to sketch, read and listen to music in my leisure time.
Source: Read Full Article
